Understanding the Meniscus: A Key Player in Knee Mechanics
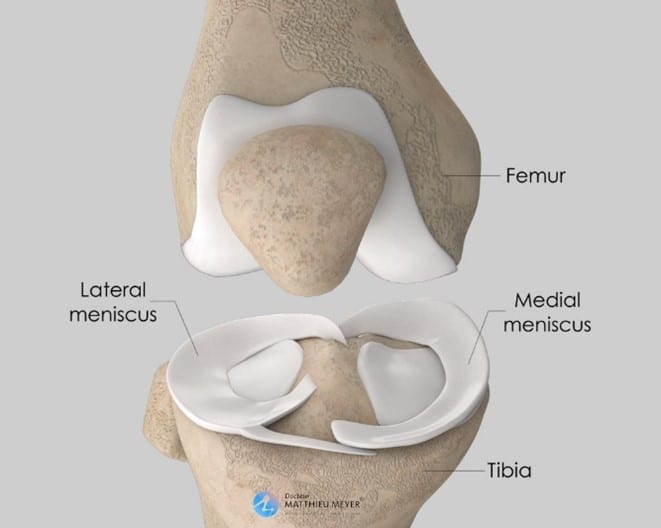
It’s a C shaped fibrocartilage that sits between the 2 knee bones (femur & tibia). There’s a medial & lateral meniscus which is perfectly concave to fit the femoral condyles snuggly in. This aids in the meniscus’ role in providing knee stability.
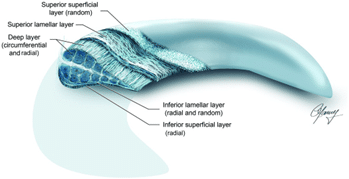
The meniscus is made up of collagen fibers, cells (glycoproteins & proteoglycans), and a very high percentage of water content (~70%). With the collagen fibers, there are 2 orientations; circumferential and radial. This is what gives the meniscus the biomechanical function to resist compression and axial loading, and aid in shock absorption. During weight bearing activities, there’s an axial load going from the femur down to the tibia. The circumferential orientation of the collagen fibres allow the force to be dissipated around the meniscus and knee joint (Calanna et al., 2022).
The meniscus receives most of its nutrients via blood flow from the genicular artery. There are 2 zones; red zone (outer third), and the white zone (inner two-thirds) (Fox et al., 2011).
Red Zone: This has very good blood supply which allows nutrients to reach the area effectively. If there were an injury in this area, there’s an increase chance of healing.
White Zone: This zone lacks direct blood vessels which makes it difficult for nutrients to reach this area. An injury here typically doesn’t heal well on its own and may need additional surgical interventions.
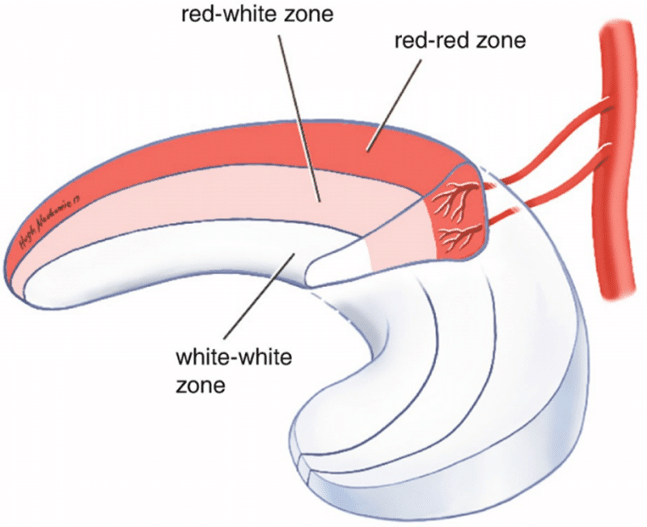
An alternative way to bring nutrition and healing factors to the areas of low blood supply is through diffusion from the synovial fluid. Synovial fluid (collection of fluid within the knee joint) acts as a lubricant and carries the nutrients to the articular cartilage and meniscus. This is why cycling is an effective exercise for meniscus tears/post op. Cycling will improve the circulation of the synovial fluid within the knee joint.
When Your Knee
Says 'Enough': Identifying Meniscus Tears
Meniscus tears can arise in many situations. It could be from heavy lifting, sudden twisting, deep knee flexion, or from an accumulation of load overtime that’s beyond the body’s capabilities. However, it’s not exclusive to athletes; they can also occur in the general population due to age-related changes in the meniscus. With age, the meniscus weakens and becomes last elastic, which increases the risk of injury.
The meniscus transmits 50% of the compressive load through the posterior knee with extension and an even greater 85% when the knees 90% flexed/bent (1). In knowing this, if you’re in the acute stage of a meniscus tear/post op, avoid deep knee flexion i.e. child’s pose, deep squats/lunges, standing quadricep stretch, sitting cross legged, etc.
If you have a meniscus tear, you may experience catching/locking, pain around the knee joint line/behind the knee, knee pain on twisting, prolonged walking/loading, deep knee flexion and sitting cross-legged.
Management Strategies for Meniscus Tears: From
Rest to Rehab
Conservative Management
By having an understanding of the anatomy and role of the meniscus, it helps guide our management. Things to modify in the first stage of rehab (0-12 weeks):
– The amount of weight bearing. Observe your current step count/running load/weight at the gym that triggers your pain, and reduce it until you find your new baseline which is pain free. From here, gradually increase the weight bearing ensuring no increase in symptoms.
– Reduce the amount of knee flexion as more force is transmitted to the posterior meniscus with greater flexion. Typically start at 45 degrees for loaded strengthening exercises, and increase progressively if there’s no pain.
– Cycle! We recommend 20 minutes moderate resistance daily to encourage nutrition from the synovial fluid. If you don’t have access to a bike, move the knee up/down whilst sitting down.
– Strengthen the surrounding knee muscles to help further offload the knee joint. If the knee is quite irritable, start with non-weight bearing ex e.g. leg extension or hamstring curls, otherwise you can go straight to weighted exercises with range or weight modifications.
– Work on improving neuromuscular control to improve your balance, and movement patterns for reduced impact on the meniscus.
Deciding on
Surgery: When Meniscus Tears Need More
a) Meniscectomy: The torn meniscus is removed.
The shock absorbing capacity reduces for those that have undergone a meniscectomy. The reduction depends on where the meniscus is and the amount removed. Research has shown larger meniscectomies lead to increase in Osteoarthritis. “Total lateral meniscectomy results in 40-50% decrease in contact area and increases contact stress in the lateral component to 200-300% of normal” (Fox et al., 2011).
b) Meniscus Repair:
Preserves the amount of meniscus available by using sutures to secure the torn edges together. This is recommended for younger patients and those where the tear is in the red zone, which enhances the chances of successful healing.
Your orthopaedic surgeon will help determine which is the best surgery option of you, if your meniscus needs be addressed surgically.
Generally, if it’s not a bucket handle meniscus tear, it can be managed conservatively first. Work with your Physio through the individualised rehab.
References:
1. Fox, A.J., Bedi, A. and Rodeo, S.A. (2011) ‘The basic science of human knee menisci’, Sports Health: A Multidisciplinary Approach, 4(4), pp. 340–351. doi:10.1177/1941738111429419.
2. Calanna, F., Duthon, V. and Menetrey, J. (2022) ‘Rehabilitation and return to sports after isolated meniscal repairs: A new evidence-based protocol’, Journal of Experimental Orthopaedics, 9(1). doi:10.1186/s40634-022-00521-8.