Shin splints aka Medial Tibial Stress Syndrome (MTSS) is a common injury and 13-20% of runners will experience it.
What is it?
MTSS can be:
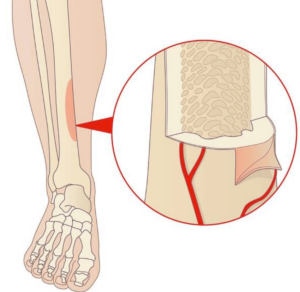
1. Caused by weakness or overuse of the tibialis posterior or soleous muscle. The muscle pulling on the bone can cause excessive traction of the tibial periosteum (the sheath surrounding the bone) which leads to inflammation. Overtime, this could lead to bone stress reaction which is a precursor to tibial stress fracture.
2. Caused by an overload to the bone. This results in microdamage and bone remodelling, which can lead to bone stress injuries and tibial stress fractures.
What are the Risk Factors?
Extrinsic factors (factors that act on the individual) are typically caused by overtraining, an arch drop (particularly the navicular), lower cadence during running, poor footwear, higher BMI, and muscle imbalances at the shin. The tibialis posterior attaches on the navicular, hence a drop in this bone during a run will contribute to an excessive traction of the periosteum.
Intrinsic risk factors (factors within the individual) include hormonal imbalances (reduced estrogen), nutritional dysregulation, osteopenia/osteoporosis, Vitamin D deficiency.
Women are 4-5x more likely to develop MTSS compared to men and it may be due to reduced bone density from the hormones. Estrogen is vital for maintaining bone health. It inhibits osteoclast activity (cells responsible for bone resorption) and promotes osteoblastic activity (bone formation). With a reduction in estrogen due to menopause or hormonal imbalances, the bone density reduces increasing the risk of stress fractures.
Inadequate nutrition also impairs the body’s bone remodelling ability. Be mindful to increase your calories in response to training load.
How do I know I have MTSS?
- Pain over the front of the shin (specifically the anterior posteromedial edge of the tibia) which typically spans over 5cm from mid to lower third of the shin.
- Pain worsening with impact/running and improves with rest. As the condition progresses, pain can persist for hours/days after the cessation of activity.
To self -assess, feel over the medial border of the distal shin bone for any tenderness. If this causes pain, you may have MTSS. Tap along the medial border of the distal shin and if there’s sharp pain along with pain on a single leg hop, you may have a tibial stress fracture.
Ok, so I have MTSS, what do I do now?
- Addressing intrinsic risk factors:
If you have any of the above intrinsic risk factors, start addressing them potentially be seeing a nutritionist, GP for blood tests to see which vitamins are lacking, and/or take supplements. - Pain management:
Oral anti-inflammatories will help reduce the inflammation and pain, and icing the area for 10 minutes post run, will help numb the pain. - Load management:
If you suspect a tibial stress fracture, rest from any impact is essential for potentially 6 weeks to allow the bone to heal. Work with your physio closely to determine when you can return to running safely.For MTSS, drastically modifying the running load/intensity for a period of 2-6 weeks may be needed but it depends on the severity. During this time, to maintain endurance, consider cross training with either the elliptical machine, biking or swimming. Once it’s largely asymptomatic for 2 weeks, gradually increase 1 variable without increasing the pain further. I.e. increase either distance, pace or frequency.
- Foot mechanics:
If there’s an arch drop when running, consider seeing a podiatrist for insoles, try low dye taping the foot with rigid tap and start on strengthening the foot intrinsics. - Gait retraining:
Cadence of < 164 increased the risk of MTSS. Try running to a metronome of 170-180bpm or listen to a 170bpm/180bpm running playlist on Spotify. Naturally, this will increase knee flexion and allow the body to better absorb the impact. - Muscle strengthening:
If you have MTSS, best to get assessed to get an individualised program for your deficits, however strengthening the below muscles is a great starting point:
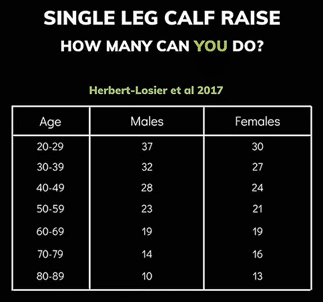
a) Calf raises biasing soleous and tibialis posterior. It’s generally the weakness/overuse of these muscles that pull at the tibial periosteum. For single leg calf raises, aim to complete 1 set of your normative value based on your sex and age (see table below). For double leg tibialis posterior, aim for 2 sets of 20 reps.
b) Hamstring and glute strengthening exercises.
The stronger these muscles, the less stress on the calf during the mid stance to push off phase of running.
c) Gluteus Medius strengthening exercises.
This reduces the chances of hip internal rotation and pelvic drop during a run, which increases the risk of MTSS.
How do I prevent MTSS?:
- Work with your running coach to ensure there’s a gradual progression in training volume & intensity. An overload from a poor structured program could lead to MTSS.
- Strengthening exercises for the lower limb especially calves.
- Wearing appropriate footwear and orthotics if needed.
- Have your running biomechanics assessed.
MTSS is a preventable and manageable condition. Understanding the underlying causes can help athletes return to their activities and reduce the risk of recurrence. Consult your physio to get your MTSS assessed and treated for a quick recovery.
References:
- Bhusari, N. and Deshmukh, M. (2023) ‘Shin Splint: A review article’, Cureus [Preprint]. doi:10.7759/cureus.33905.
- Luedke, L.E. et al. (2016) ‘Influence of step rate on shin injury and anterior knee pain in high school runners’, Medicine & Science in Sports & Exercise, 48(7), pp. 1244–1250. doi:10.1249/mss.0000000000000890.
- Menéndez, C. et al. (2020) ‘Medial tibial stress syndrome in novice and Recreational Runners: A systematic review’, International Journal of Environmental Research and Public Health, 17(20), p. 7457. doi:10.3390/ijerph17207457.